Toileting transfer remains one of the most frequent, urgent, and least discussed moments in care.
Every toileting-related fall, every strained back, every moment of lost privacy asks the same questions:
Are people happy with their toileting transfer assistance now?
Are staff happy with the equipment they are asked to use for toileting transfer?
Are families happy with the dignity of their loved ones who depend on assistance for toileting transfer?
The People Behind PPAL®
Together, these contributors represent both the human heart and research discipline behind the PPAL effort.
The PPAL story started around a dining room table — a small group of family, friends, and colleagues who saw the same problem and believed in a safer, more dignified solution. Without their support, this would not be possible.
They became the seed funders, advocates, and early testers who turned a personal challenge into a national movement for reform.
Today, PPAL’s advisory network includes leading experts in:

Rehabilitation Engineering
Human Engineering Research Laboratories (HERL), VA Pittsburgh

Safe Patient Handling & Mobility
National leaders in fall prevention and ergonomic care

Nursing & Rehabilitation Science
Researchers focused on dignity, independence, and safety in daily care
Industrial Design
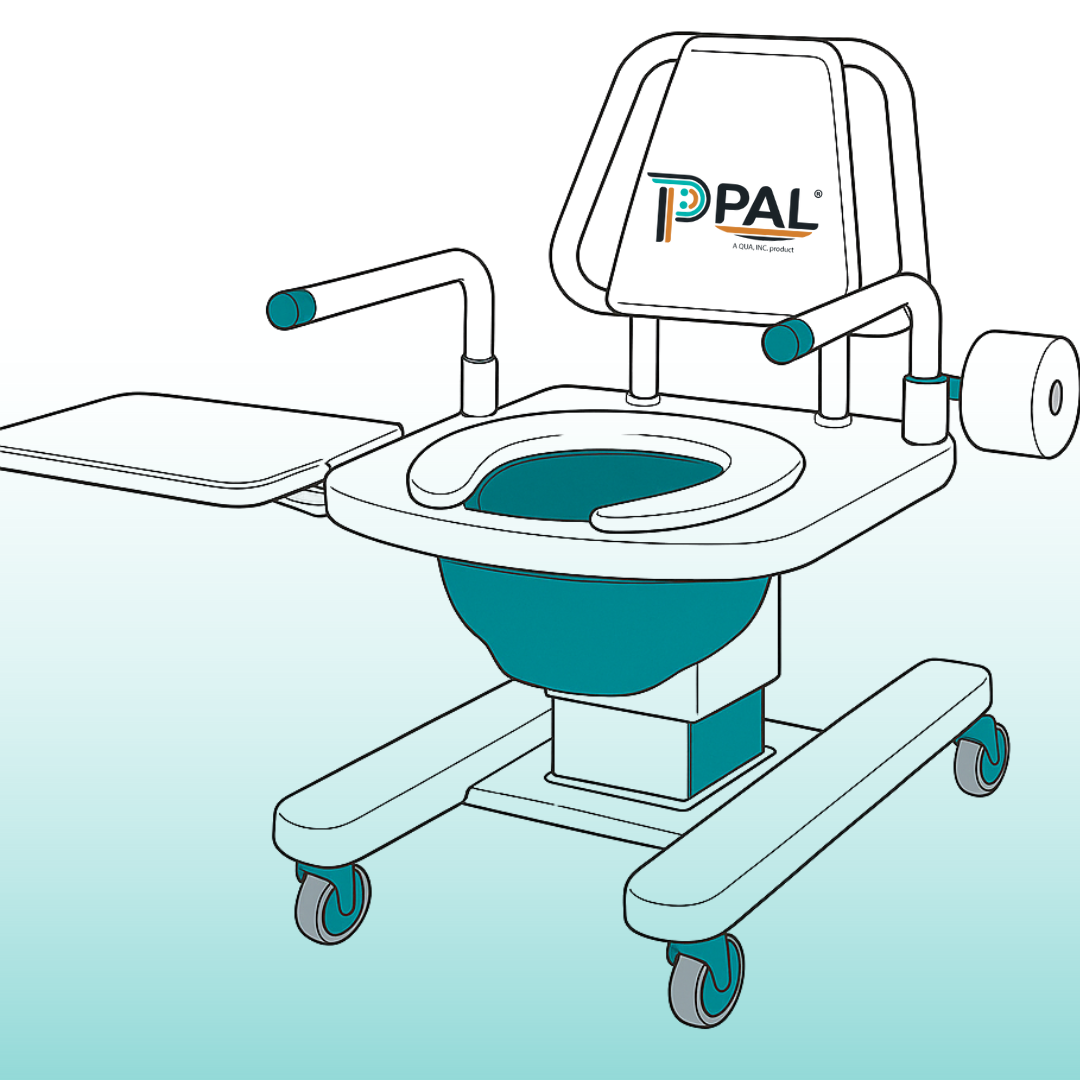
Paul Carlson, Brownlie Design – Co-designer of the PPAL prototype
Built Out Of Lived Experience
Founder Story
I came to care about toileting transfer out of lived experience. My mother lived with post-polio syndrome and refused to give up her independence. Every traditional option — briefs, bedpans, slings — in her mind – compromised her dignity. Her choice was to self-transfer onto a traditional bedside commode – which required help from her children.
After she passed away, My family felt that something different was needed. Something that would make transfers safe, predictable, and dignified.”
– Peg Graham, Inventor and CEO, QUA Inc.

PPAL is about reform — improving what is
available now with safer, smarter, more dignified design.
Why Does It Matter: It’s because right now
- 45% of inpatient falls happen during toileting (Hitcho et al., 2004; Cameron et al., 2018).
- Data about toileting-related falls in nursing homes is almost non-existent
- Caregivers experience preventable back injuries from repeated manual transfers (Nelson & Baptiste, 2004).
- Workers often don’t use the lifts provided (Khairallah et al, 2024)
REFORM IN ACTION — THE PPAL DIFFERENCE


What if a Toileting Transfer Device were to:
- Empower Toileters — to safely contribute to their own transfers.
- Prevent injury — reduced lifting strain, and eliminated unsafe workarounds.
- Protect dignity — designed for a private act of care with compassion and control.
- Deliver ROI — reduces costs of staff injury, insurance settlements, improves quality of care, reduces staff turnover linked to unsafe toileting.
RESEARCH AND REFLECTIONS
FROM THE FIELD
Toileting safety isn’t a side issue — it’s a mirror of how care is delivered.
Our insights connect lived experience, clinical data, and practical reform.
We talk about falls — but often avoid the toileting transfers underneath them. When we treat these moments as “accidents,” we miss the patterns we can change.
Reform, not disruption: dignity is non-negotiable, independence is supported, time is safety, and aides deserve protection.
Medicare already measures toileting transfer independence. When it’s visible, it becomes a priority — unlocking training, time, and investment in safer systems.
Toileters aren’t one demographic — they’re anyone whose body, environment, and timing don’t line up safely, especially when urgency, privacy, and risk collide.
STAY CONNECTED
Follow PPAL® on LinkedIn and Facebook for insights on dignity, safety, and smarter systems of care—plus updates on advocacy, progress, and impact.
Join the conversation. Stay informed. Be part of the change.