We talk about falls. But a major reason for falls —toileting assistance—is often left unspoken. Every toileter faces it daily. Every aide, whether paid staff or loving family member, manages it repeatedly. And for many, it’s the moment where independence and dignity feel most at risk.
Let’s talk about how we approach toileting transfers for older adults and those with physical disabilities.
PLEASE NOTE: Research reported in this publication is funded by the National Institute Of Nursing Research of the National Institutes of Health under Award Number R44NR019516. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Why Toileting Transfer Matters More Than We Admit
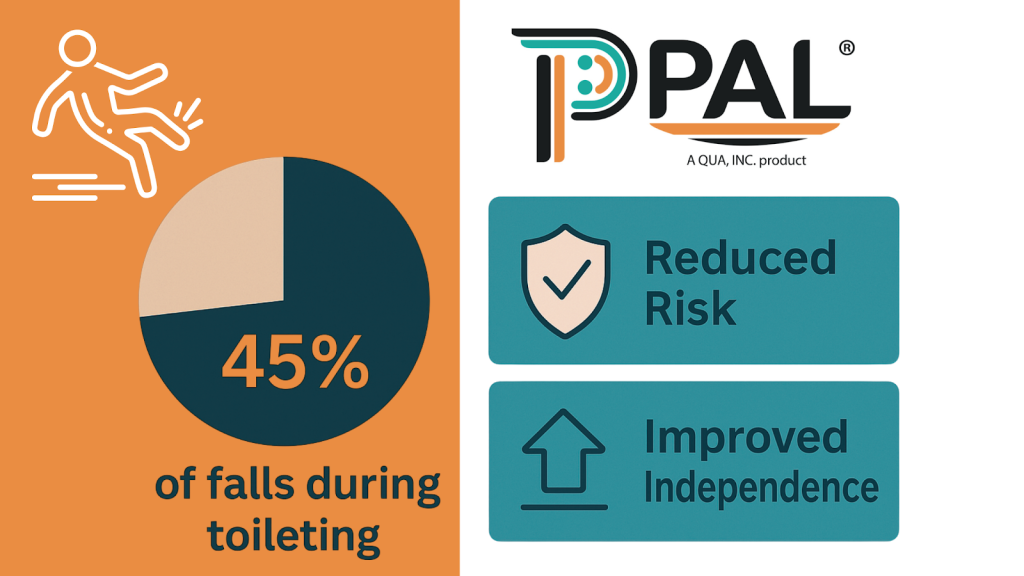
Toileting transfer is frequent, urgent, and private. Most adults urinate 4–10 times a day (Wyman, 2022) and have a bowel movement up to 3x daily or at least 3x/week (Walter, 2010). That urgency doesn’t pause for staff shortages or shift changes. When help is delayed, toileters often try to manage on their own. These “I’ll do it myself” moments are a leading cause of falls during toileting, which account for up to 45% of inpatient falls (Hitcho et al., 2004; Cameron et al., 2018).
Reform, Not Disruption
The answer isn’t to tear down systems but to reform them. That means improving what we already do with a sharper focus on dignity, independence, and timeliness.
Four principles guide reform in toileting care:
- Dignity is non-negotiable. Toileting is the last true frontier of privacy. Solutions must protect autonomy, not strip it away.
- Independence matters. Independence doesn’t mean “alone”—it means supported. With the right design, toileters can participate safely in their own transfers.
- Time is safety. Every delay stretches risk like a rubber band. Fall protocols must account for toileting urgency, not just gait or balance scores.
- Aides need protection. Safer systems reduce back injuries, burnout, and turnover. Staff deserve dignity too.
Where Innovation Fits
If toileters are engaged in their own transfers, they could reduce the need for strenuous lifting and restore a measure of their own privacy. This won’t replace caregivers or clinical judgment. Instead, it could make it easier to consistently do the right thing: safe, dignified toileting that works for both toileters and aides.
Evidence supports this approach: finding targeted interventions likely to be more effective than generic fall prevention programs (Cochrane Review, Cameron et al., 2018). Toileting transfer is our targeted, high-frequency risk—addressing it directly can yield measurable improvements in safety and satisfaction.
A Call to Measure What Matters
Healthcare loves dashboards, but toileting is rarely tracked. That silence hides risks, costs, and opportunities for improvement. As CMS ties reimbursement to preventable falls , reform starts by naming the gap: toileting transfer must be measured and managed to optimize functional outcomes.
Moving Forward
Toileting transfer doesn’t have to be the moment where dignity and safety collide. By reforming our approach—prioritizing dignity, designing for independence, treating time as safety, and protecting staff—we can transform this everyday act into something safer, calmer, and more human.
Because dignity isn’t optional. It’s the foundation of care.


