Who Pays for Toileting Transfer Safety — and Why It Matters to Toileters
If you’re a toileter — a person who needs help getting on and off the toilet — reimbursement probably feels distant, abstract, or irrelevant. It can sound like something that only administrators, insurers, or policymakers worry about.
But reimbursement quietly shapes almost everything about how toileting transfers are handled.
It influences what gets measured.
What gets trained.
What gets invested in.
And what quietly remains invisible.
Here’s the plain-language reality:
- When something is measured, it becomes visible.
- When it’s visible, it becomes a priority.
- When it’s a priority, it gets resources—time, training, staffing, equipment, and safer systems.
Toileting transfers ARE measured – by Medicare. But are they a priority for Skilled Nursing Facilities, Home Health Agencies? Not yet. We aim to change that.
How reimbursement actually shows up in real life
“Reimbursement System” is the term used for the complicated way Medicare pays money to skilled nursing, home health agencies, in-patient rehab and long-term care hospitals (“post acute care providers”). You get an Explanation of Benefits that reflect thousands of dollars being paid. You don’t get that money, you may own co-insurance. Tons of regulations creates “rules of the road” that these “providers” have to pay.
Reimbursement shapes care environments in very real ways.
It shows up as:
- Quality metrics: If providers believe that something impacts the quality of care, it gets documented, audited, and discussed in leadership meetings.
- Pressure around “avoidable events”: Medicare believes falls and injuries don’t have to happen if providers do the right thing – so providers work hard to reduce falls or injuries.
- Equipment purchasing logic: Providers invest in what they think will help them provide high quality care or prevent falls/injuries– but they struggle to choose which new “thing” to spend money on
This helps explain why toileting transfers have remained stuck. Toileters know that the risk to quality and safety is real, but leadership doesn’t “see” that yet. That means that toileting transfers are not yet targeted for investment.
Medicare & Toileting Transfers: “Independence Score”
But guess what? Medicare DOES track Toileting Transfers.
It is buried deep within the reimbursement system.
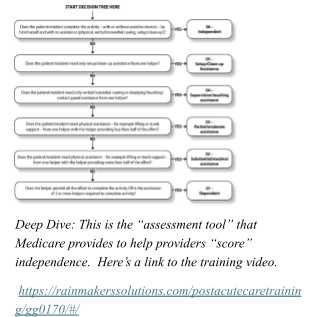
Medicare requires providers to document your toileting transfer independence as part of the clinical assessment tools used to collect reimbursement. The tools have different names for each kind of provider, but they all “score” toileting transfers in the same way – see the “Deep Dive”
- Minimum Data Set (MDS) in skilled nursing facilities
- Outcome and Assessment Information Set (OASIS) in home health agencies
- Inpatient Rehabilitation Facility Patient Assessment Instrument (IRF-PAI) in rehab hospitals
- Continuity Assessment Record and Evaluation (CARE) in long-term care hospitals
The scores are used for care planning, quality reporting, and Medicare payment classification.
The “Independence Score,” can be used by providers to determine if their Toileters can toilet:
With dignity — privacy respected, no unnecessary exposure of “private parts”
With independence – maintaining pride in “doing for oneself”
Safely — reduced fall risk, reduced toileter and staff injuries
Appropriately supported — the right help, at the right time, in the right way
Avoiding unnecessary strain on staff — at protect aides as well as toileters
The goal isn’t to add paperwork. The goal is to redefine what toileters’ “good care” looks like.
When toileting transfers are counted as part of independence, they stop being invisible. They become a measurable quality moment—one that providers can justify investing in.
What changes when toileting transfers are made visible
When toileting transfer independence is recognized as “Quality” :
- Providers have more effective and efficient tools and processes
- Staff know that they are delivering the highest quality of care
- Toileters are less likely to feel rushed, ignored, or unsafe
- Care shifts from reaction to prevention
Most importantly, dignity stops being something people hope for and starts being something systems are designed to protect. Many providers genuinely care about resident experience, staff safety, and organizational values that prize toileter independence. But in the real world operations, as we all know, financial alignment determines whether a good idea becomes a standard practice or stays a passion project. In future blogs, we’ll explain how safe Toilet Transfers help providers’ financially.


